Ever seen the film Children of Men? (if not go and watch it, it’s great)
In it mankind has been struck down by the inability to reproduce. Babies are no longer born and it sends the world into meltdown.
It’s not looking so much like science fiction anymore…
In perhaps the most chilling study I’ve read in recent times and one which certainly matches my own personal struggles and what I see in many of the clients I work with, researchers have shown that over the period from 1987 – 2004, comparing men of the same age, testosterone levels dropped by 17%.
(I’ve included a copy of the study below for those who want to read it)
If we carry on at that rate we will be looking at a sterile population somewhere around the middle of the century.
“But Low T is something which only happens to out of shape guys, isn’t it?”
Not so…
When I hit my lowest T levels ever and was struggling with zero libido, erectile dysfunction and general apathy about life…I was in great shape to look at, super low body fat and well defined musculature, it was just on the inside it was all going wrong…
Believe me when I say this is a problem which can affect us all, and it is…
Personally I believe it is the unspoken epidemic of the 21st century. When I dig down with any of my male clients (and a lot of my female ones) this is pretty much ALWAYS a problem they have…it’s just it’s never spoken about, especially amongst men, and women don’t often consider it as even a potential problem.
Testosterone (for both sexes) does a huge amount more than just help us have better sex. It’s hugely important for mood, depression, confidence, lust for life, muscle growth, youthfulness…in short life’s a lot better with higher levels of testosterone, for both men and women.
Yup, women need testosterone too, not in anywhere near the quantities which men do, but if women have low libido, apathy or any of the issues mentioned above, one of the first places I look is their T levels.
Now, I don’t want this post to be all doom and gloom so I want to give you the good news. This is all easily reversible without needing hormone replacement therapy.
The first thing I would do is go and get your Vitamin D levels checked. When you come back as deficient (I almost guarantee you will) start to get 20 mins full body sun exposure a day, without suncream or sunglasses, (you may need to build up to this to avoid getting burned). In addition or instead (if that’s just not possible), start taking a quality Vitamin D3 supplement.

Vit D is where Testosterone production starts and often just getting more of this will make a noticeable difference. Make sure to get a good quality supplement which also contains Vitamin K2. Vitamin K2 is essential in combination with Vitamin D (especially in the quantities we’re going to be taking it! as it ensures it gets to the right places.
Now the key here is the dose. You should be taking at least 10000 iu, if not 20-30,000 iu a day!
That’s a lot of Vitamin D, but it’s these quantities which will start to make a dent in the problem. Ideally do it before bedtime, with a bit of melatonin as Vitamin D can affect sleep. If you find you can’t sleep, no problem, just do it first thing in the morning and it’ll still do its job.
Do this for a few weeks and then go and get your levels retested. Make sure you get tested as Vitamin D toxicity is a thing and you want to ensure you are on top of it. If you are still low, wait a couple of weeks and then repeat until you are registering at the very high end or at least slightly above of the normal Vitamin D ranges. I would be aiming for at least 80 nmol.
Now this isn’t a panacea and there are a tonne of other things you can be doing to boost the Big T. A lot of them lifestyle related:

- Life heavy weights
- Eat properly
- Get plenty of sleep (testosterone is created while you sleep)
- Reduce stress
This last one is particularly important as testosterone is created from the same building blocks as cortisol. If you’re highly stressed, all the resources which could be creating testosterone will instead be going into creating cortisol, meaning there’s none left over to create testosterone.
Added to that, there are a tonne of natural supplements we can be using to help with this situation as well.
The long and short of this?
I’ve built protocols using these foundations with clients and have several 55-60 year clients who are maxing out their testosterone levels without having to use hormone replacement therapy and feel (and look!) absolutely great as a result (and their relationships are much better as well!).
The study:
Travison, TG, AB Araujo, AB O’Donnell, V Kupelian, JB McKinlay. 2007. A population-level decline in serum testosterone levels in American men. Journal of Clinical Endocrinology and Metabolism 92:196–202.
In one of the largest study of its kind, Travison et al. report a population-wide decline in Massachusetts’s men’s testosterone levels during the last 20 years that is not related to normal aging or to health and lifestyle factors known to influence testosterone levels.
They found that testosterone concentrations dropped about 1.2% per year, or about 17% overall, from 1987 to 2004. The downward trend was seen in both the population and in individuals over time.
The decline is consistent with other long-term trends in male reproductive health, including decreases in sperm quality and increases in testicular cancer, hypospadias and cryptorchidism.
The strongest association was observed in same-aged men from different sampling years.
For example, a 65-year-old in 2002 had lower testosterone levels than a 65-year-old in 1987. Lower concentrations of testosterone can increase a man’s risk for age-related diseases, depression and infertility.
Also, the younger and older men in the study experienced similar hormone declines that dropped faster than would be predicted by normal aging.
Context: In men, the hormone testosterone guides behavior and reproduction. It controls growth and development of sex organs and other typically male characteristics, such as facial hair and a deep voice.
Normally, levels fluctuate from conception through puberty then level out during adulthood before declining as men age. Some chronic health problems typically seen in older adults, such as diabetes, depression and obesity, are associated with lower testosterone levels.
Recent studies have that found environmental impacts on testosterone levels. For example, testosterone levels were lower in US Air Force veterans exposed to dioxins while spraying Agent Orange during the Vietnam War, as well as in men exposed to phthalates at work.
What did they do? Travison et al. used blood hormone data and personal information collected from men living in Boston, MA, as part of the Massachusetts Male Aging Study (MMAS). The MMAS examined men’s health and endocrine function. Data were gathered during three home visits from 1987-89 (T1), 1995-97 (T2), and 2002-04 (T3).
Total testosterone (TT) and serum sex hormone-binding globulin were measured in the blood and available testosterone (BT) was calculated. The men self-reported such things as basic demographics, health status, and smoking and alcohol use.In this study, Travison et al. analyzed data from 1,532 men (1,383, 955, and 568, respectively, from T1, T2 and T3) that met age and birth year requirements. Participants ranged from 45 to 79 years old and were born between 1916 and 1945.
The researchers excluded high and low T levels, missing data, and unidentified prostate cancer treatment. Within the sample, they calculated and compared three separate but related associations among concentration, age, and time. They looked at changes in testosterone concentrations in the group of men at different years and ages associated with T1, T2, and T3; testosterone declines in individual men as they aged during the study; and testosterone concentrations of men of the same age but in different years (age-matched).
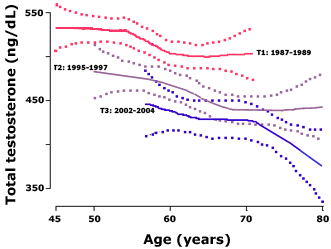
What did they find? Travison et al. found strong evidence of a decline of more than 1% per year in men’s blood testosterone levels during the last two decades. The graph (above) shows average levels for each for men of different ages in each of the three measurement periods (T1-T3).Dotted lines are 95% confidence bands. Adapted from Travison et al.
The first comparison to make is that within a cohort, older men tend to have lower testosterone levels. Compare, for example, 80 yr old men in T3 compared to 60 yr old men.The crucial comparison to make is from one cohort to the next, comparing men of the same age. For example, 60 yr old men during the first measurement period (red line, 1987-1989) had total testosterone levels over 500 ng/dL.
Men aged 60 yrs old in the third cohort (blue line, measured 2002-2004) had TT below 450 ng/dL. There is no overlap between the confidence bands of T1 vs T3: T3 (measured 2002-2004) is always lower than T1.The trend holds regardless of the men’s age.
Similar declines over the 17 years were seen in all ages of men in the study.Travison et al. note that the decline within the cohorts related to age is less than the decrease observed across cohorts. For example, men aged 70 in T1 had TT only 6% less than men aged 45 in the same cohort. But 60 yr old men in T3 had TT concentration approximately 13% lower than men the same age in T1.
To illustrate this point another way, Travison et al. compared the average decline of testosterone levels in T1 vs T2 as a function of age, and then contrast that with differences in testosterone between men of the same age in T1 vs T2. Note that T1 and T2 were only separated by 9 years.
The average declines in T1 and T2 per decade of life were 17 and 20 ng/mL, respectively. But 65 yr old men in T2 had total testosterone levels 50 ng/mL lower than those in T1, even though the samples were separated by less than a decade.Travison et al. then estimated the decline over time, from the first cohort to the third, for men of the same age (what they called the age-matched decline).
They found that testosterone declined by 1.2% per year (95% CI 1.0% to 1.4%).
Bioavailable testosterone (BT) also showed similar declines over time. The strongest associations again held for age-matched trends with declines of 1.3% per year (95% CI 1.7% – 1.1%).
None of the health and lifestyle factors examined were associated with either age-matched declines in either TT or BT: The age-matched declines remained essentially the same after controlling for chronic illness, general health, medications, smoking, body mass index, employment, marital status, and other indicators.Finally, the trends held when analyzing the data in a number of different ways, including by interview date, study cohort, restricting to men of certain ages or birth cohorts, and considering incomplete versus complete data.
What does it mean?
Travison et al. find that testosterone levels declined in Massachusetts men by approximately 1.2% per year from the late 1980s through 2004, controlling for the age of the men and other possible confounding variables.This study is important because of its large sample size and long duration. Few studies have looked directly at testosterone levels over time.The results are surprisingly consistent with another set of long-term human epidemiology studies. Those studies also show a long-term decline in male reproductive functions, such as decreased sperm health and increased infertility, which are highly associated with or controlled by testosterone and other androgen hormones.
The rate of decline reported in this study is roughly comparable to the rate of decline of sperm count reported first by Carlson et al. in 1992 and then reanalyzed by Swan et al.in 2000.In commentary accompanying Travison et al.’s study in the Journal of Clinical Endocrinology and Metabolism, Dr. Shalender Bhasin (Boston Medical Center) writes: The data in this study are “important because they provide independent support for the concerns raised earlier about the reproductive health of men.” … “it would be unwise to dismiss these reports as mere statistical aberrations because of the potential threat these trends– if confirmed– pose to the survival of the human race and other living residents of our planet.”